Your Most Common Mastitis Questions Answered- Everything You Need to Know About Mastitis
Read time | 20 min
Mastitis is a moderately common breast condition that, despite its familiarity, remains quite a mystery. The lack of clarity surrounding mastitis may be in part due to the ever-expanding knowledge on the condition, changing and varied theories regarding its causes, the wide range of clinical symptoms, or a large number of providers and clinicians who observe it in lactating and non-lactating patients.
The potentially conflicting information given to lactating parents leaves them without clear answers, thus resulting in lingering questions. Adding to the confusion, there is a shortage of in-depth information geared towards parents regarding mastitis. My goal with this post is to answer the most common questions parents have and provide a resource for anyone looking to get more than just a basic understanding of this often difficult to understand topic.
Mastitis can develop at any time in a person's life, regardless of if they're currently lactating or not. Lactational mastitis- the focus of this post- generally occurs in one breast only. I will briefly touch on bilateral (both breasts) mastitis at the end of this post.
Note: There’s a lot of information in this post. Use the table of contents or Search your question using CTRL/ CMD F to quickly get to the information you’re most interested in.
Defining Mastitis
There are varying definitions of mastitis that you might encounter. I've attempted to provide clarity by defining the most common terms.
Important Mastitis Terminology
Acute Mastitis: An inflammatory condition of the breast caused that may or may not be caused by a bacterial infection
Inflammatory Mastitis: A redundant term used to describe non-infectious mastitis- that is, mastitis symptoms caused by milk stasis rather than bacteria.
Infectious Mastitis: A term used to describe mastitis caused due to a bacterial infection of the breast.
Adenitis: A sub-distinction of Acute or Subacute Mastitis thought to refer to inflammation of the mammary gland due to blocked ducts with less severe symptoms- usually only needs first-line treatment and may not need antibiotics
Cellulitis: A sub-distinction of Acute or Subacute Mastitis thought to refer to an infection of the interlobular connective tissue. It generally requires antibiotics or equivalent treatment. There is some disagreement as to whether Cellulitis, which is a condition in its own right, is actually mastitis.
Subclinical Mastitis: A breast infection without any accompanying clinical symptoms typically associated with Acute Mastitis
Subacute Mastitis: A contentious term borrowed from the dairy industry to describe mastitis that as local symptoms but without any of the systemic symptoms. May be referred to as Mammary Dysbiosis.
Suppurative Mastitis: An infection of the breast which causes the production of pus
Plugged duct: A painful but non-infectious condition of the breast caused a blocked milk duct. Mild systemic symptoms, such as fever and flu-like symptoms, may accompany plugged ducts (as inflammatory mastitis), and It can progress into infectious mastitis if milk flow is not restored.
Mammary Dysbiosis: The altering of the breast microbiome ( the community of organisms of the breast) by an overgrowth of opportunistic bacteria and a biofilm formed by the bacteria, which causes a decrease in commensal (normal/healthy) bacteria.
Milk Stasis: A buildup of milk within the mammary gland
Breast Abscess: A collection of pus that forms in a contained pocket inside the breast
Nipple Bleb: Blockage of a nipple pore that may appear like a pimple on the face of the nipple and may cause significant pain (sharp, stabbing) during feeding.
Who is Prone to Mastitis?
You're more likely to develop mastitis if you have had previous bouts of mastitis, are immuno-compromised (such as having uncontrolled diabetes or Lupus), or are suffering from a chronic illness.
Mastitis risk factors include:
Infrequent or insufficient milk removal
Being less than six weeks postpartum
Oversupply
Direct breastfeeding a baby whose nose and throat are colonized with S. Aureus
Pumping
Nipple damage or trauma
Plugged ducts
Prelacteal feeds
Delayed initiation of breastfeeding/milk expression
Nipple shield use
Stress/Fatigue
A period of extended pressure of the breast such as an ill-fitting bra, belly sleeping, etc
What Causes Mastitis?
The exact causes of mastitis are still poorly understood; however, the two most accepted explanations are 1) inflammation due to infrequent or inadequate milk removal and 2) the introduction of pathogenic bacteria through nipple wounds or nipple pores.
There is a correlation between weaning or increased supplementation and mastitis when frequent milk expression is not maintained.
There is also a correlation of mastitis cases in those with overabundant supplies or those who have babies with feeding difficulties (such as tongue-tie), resulting in insufficient breast drainage.
Inflammatory mastitis is thought to be caused by the opening of junctures between lactocytes (milk-making cells) in the mammary gland. The build-up of milk in the glandular tissue and the resulting juncture openings allow milk components (such as cytokines) to leak into the surrounding breast tissue, causing inflammation.
Which bacteria cause Mastitis?
There's a variety of bacteria that have the potential of causing an infection that is present in the typical microbiome of the breast. In other words, the presence alone of the following bacteria in your milk isn't an indication of an infection, explaining why symptoms are most often used to diagnose mastitis rather than milk cultures.
S. Aureus
S. Epidermis
S. Marscens
E. Coli
Gram-Negative Staph
Group A Strep
Psuedonomas
Whether or not the introduction of pathogenic bacteria not usually found in the breast microbiome is alone enough to initiate mastitis symptoms remains to be seen. Still, new evidence is emerging that a critical component to both acute and subacute mastitis is a decrease in the number of certain bacteria. Interestingly, some research also shows that in cases of both subclinical and acute mastitis, there may be a correlation between an increase in aerotolerant bacteria (bacteria that can tolerate oxygen) and a reduction of obligate anaerobes (bacteria damaged by oxygen).
S. Aureus, S. Epidermis, and Pseudomonas may be the most common bacteria genera that cause mastitis, with S. Aureus responsible for most acute mastitis cases and S. Epidermis for subclinical cases.
Where does Mastitis start?
Infectious mastitis generally starts by entering through a nipple wound or via the nipple pores. It can also begin in the breast from prolonged milk stasis, though the mechanisms by which that occurs is still unclear.
Non-infectious mastitis (solely inflammation) begins in the breast, typically due to a blocked milk duct or inadequate milk removal.
Because the majority of breast tissue is on the outer quadrant of the breast (same side as your armpit), the incidence of mastitis occurring there is higher compared to other parts of the breast (under your breast, for example).
Can one have mastitis without infection?
Yes, you can have mastitis in the absence of infection or the absence of clinical signs of infection, such as subclinical mastitis. Subclinical mastitis may be more common than we realize, but our bodies manage the infection without it progressing to acute mastitis.
Mastitis without infection may quickly be resolved and may not require antibiotics.
Signs & Symptoms: What does Mastitis Look Like?
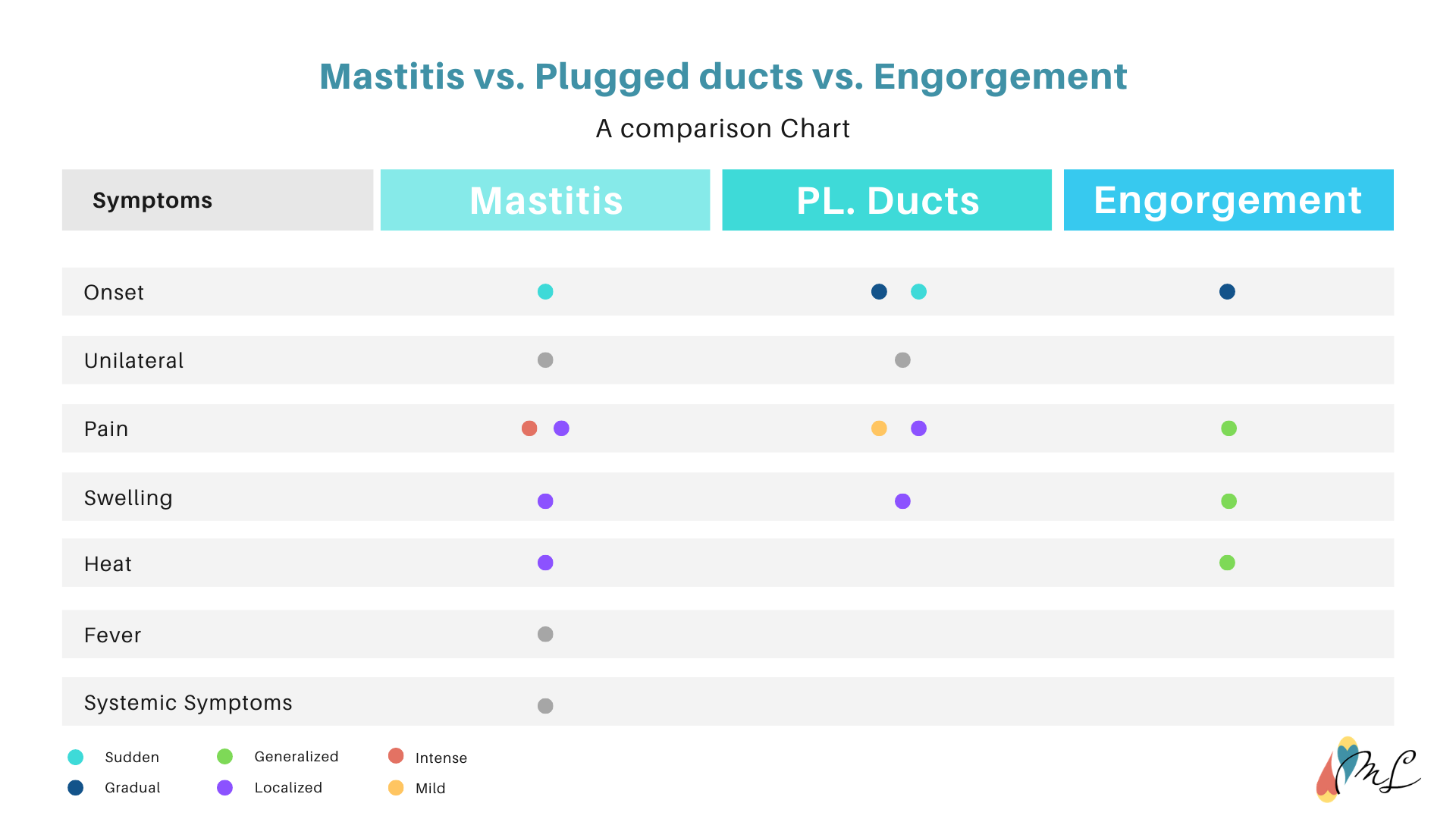
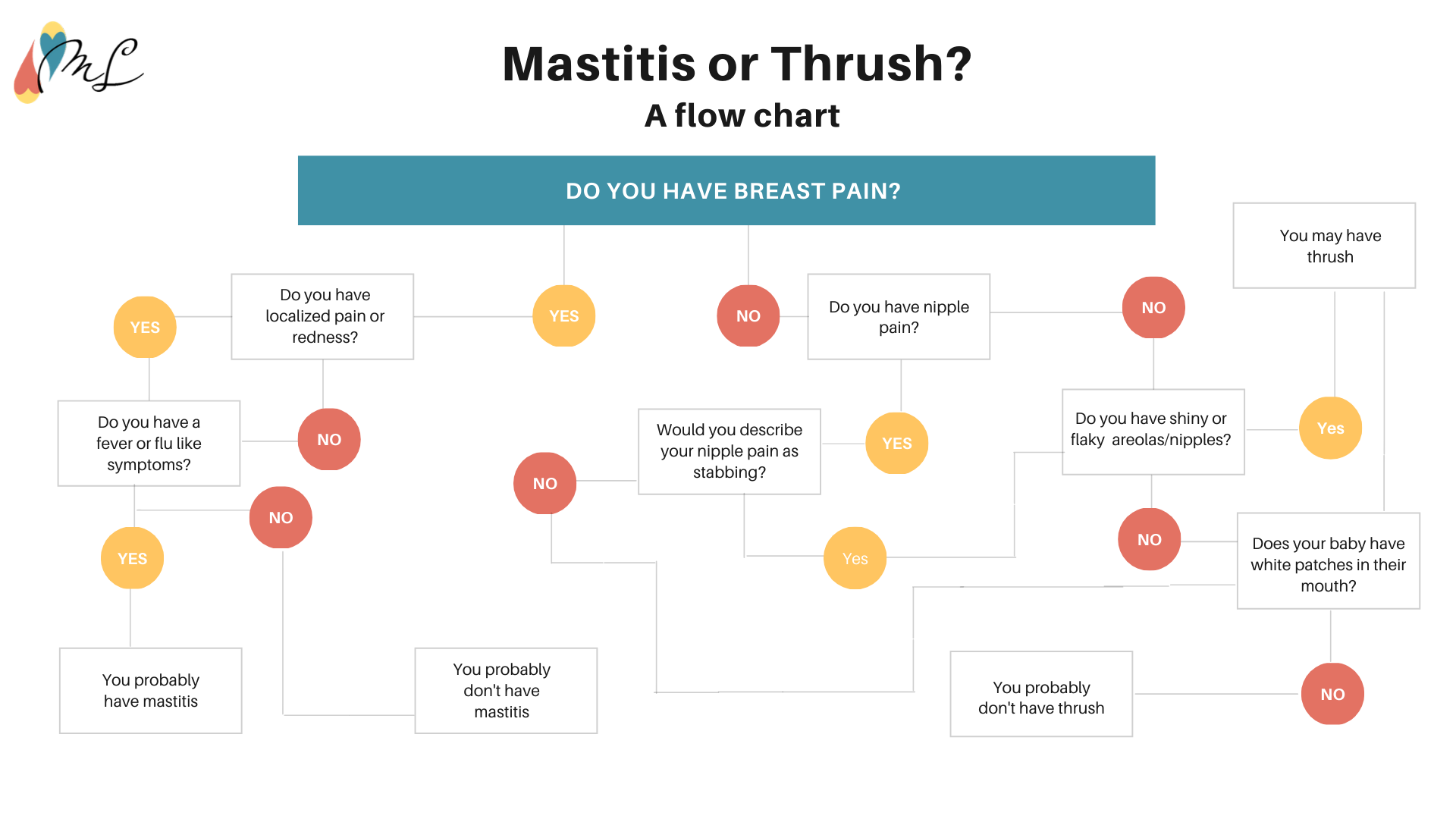
The diagnosis of mastitis is generally reached if you have two or more localized symptoms as well as at least one systemic symptom. Lactation-related Mastitis typically only affects one breast.
Local symptoms may include:
A tender, hot, painful area on the breast
Localized redness or red streaking
Localized firmness or swelling
Swollen Auxillary (armpit) lymph nodes on the respective side
Pain with breastfeeding or expressing
Clumpy or gelatinous milk
Pus or blood in milk
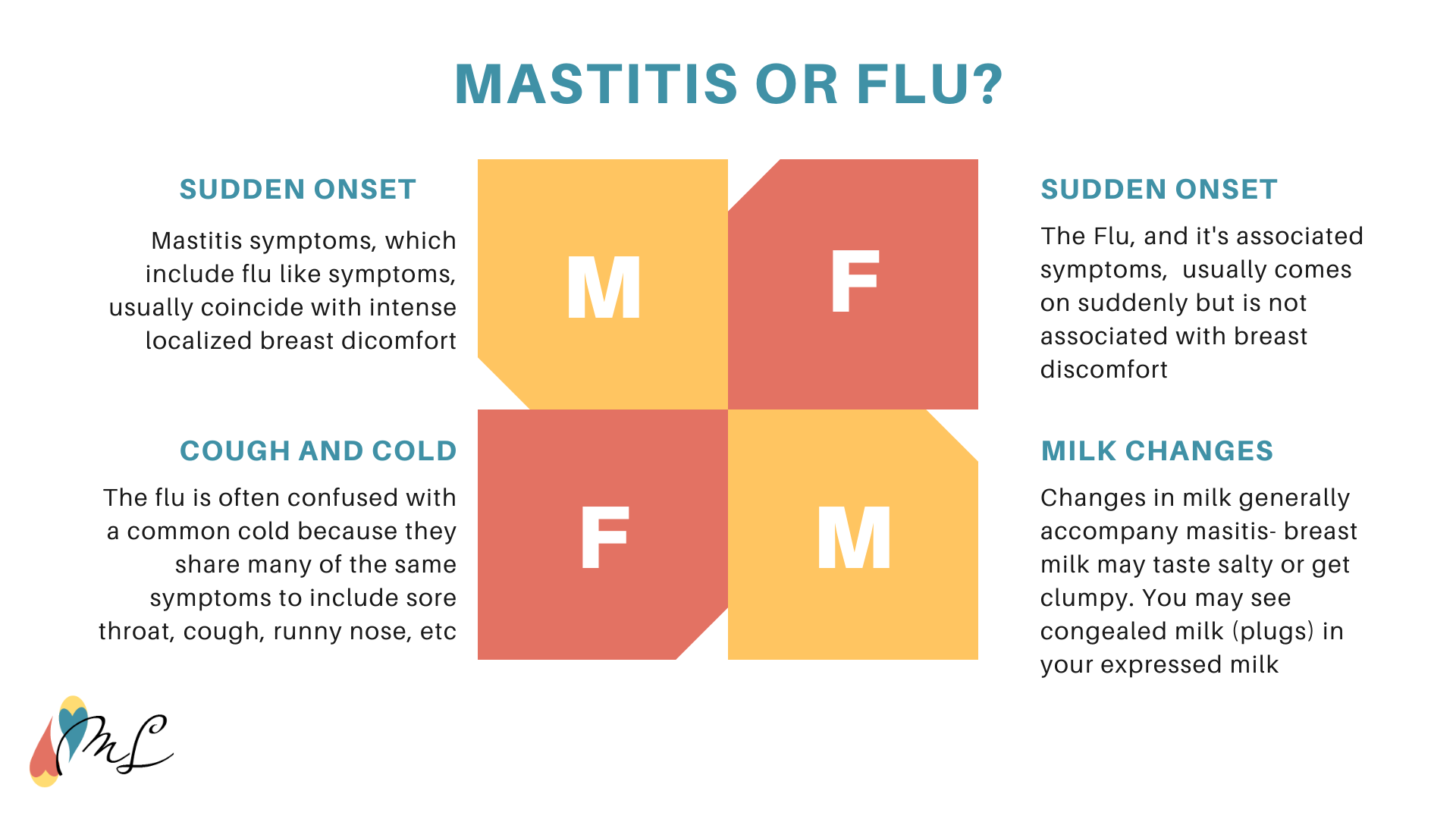
Systemic Symptoms may include:
Fever (101 or higher)
Chills
Headache
General discomfort or feeling sick (Malaise)
Nausea
Muscle Pain (Myalgia)
Decreased energy (Lethargy), Fatigued
Systemic symptoms may precede breast discomfort or may develop after your breast symptoms appear, and fever may be present even in cases of inflammatory mastitis.
What does Mastitis feel like?
Because Acute mastitis is diagnosed based on physical and systemic symptoms- both of which are unpleasant- I would venture to say that mastitis feels terrible. More discomfort usually accompanies mastitis compared to plugged ducts and engorgement, but in cases of subclinical mastitis, you may not feel anything at all.
Despite pain being subjective, many parents describe mastitis as excruciatingly, exceptionally, or intensely painful.
Why is Mastitis so painful?
Mastitis is painful due to the Inflammation process. Inflammation sends out chemicals in an attempt to protect, defend, and heal damaged cells or pathogens which stimulate nerves and leads to swelling (buildup of fluid between cells), which may further exacerbate your discomfort.
Inflammation is also responsible for the other symptoms- all of which are byproducts of the healing process.
Anti-inflammatories and pain medication can help ease discomfort, and there is a wide variety of medications that are safe to use while breastfeeding. Many parents choose to use Ibuprofen, which is both an analgesic (pain reliever) and anti-inflammatory and is compatible with breastfeeding.
Can you get Mastitis near your armpit?
Due to breast anatomy, very rarely mastitis may occur near or in your armpit in an area of the breast called the tail of Spence. It's more common for parents to confuse engorgement or milk stasis in the mammary tissue as mastitis, especially since both can cause moderate discomfort. Treatment for mastitis, should it occur in the tail of Spence, would be the same for mastitis located in other parts of your breast.
Is mastitis contagious?
Mastitis and it's accompanying symptoms are not contagious, and milk from mastitic breasts is safe for your baby to ingest. Rest is encouraged to help speed recovery, but isolation is not necessary, and nobody can catch mastitis from being exposed to someone who has mastitis.
Can mastitis occur without redness, flu-like symptoms, or pain?
Mastitis can present without flu-like symptoms and moderate discomfort (such as with subacute mastitis) or any of the typical mastitis symptoms, as is the case with subclinical mastitis. For some parents, the only sign of subclinical mastitis is milk that clumps after expression.
With that said, if you're experiencing only moderate discomfort and or a lump/wedge without redness, heat, or systematic symptoms, other possibilities such as plugged ducts should be explored first.
Getting a Diagnosis- Testing for Mastitis
Who to call/see for Mastitis?
Many parents are unsure of who to call when they suspect mastitis, especially since they are so many providers who are capable of providing guidance. If severe systematic symptoms have not developed or been present for longer than 12-24 hours, calling a local IBCLC to help you resolve the issue is an excellent first step. Otherwise, you can visit their primary care provider, family doctor, or OBGYN.
If you become very ill or are unable to get seen quickly by your provider, you should seek care from urgent care or the ER.
Who can diagnose Mastitis?
Contrary to popular belief, lactation professionals, including International Board Certified Lactation Consultants (IBCLCs), can not formally diagnose Mastitis. Only medical doctors can provide a formal diagnosis, and only they can determine which, if any, antibiotics are needed.
With that said, despite not being able to diagnose mastitis, IBCLCs are able to assess and help you manage mastitis before, during, and after the use of any antibiotics. Many IBCLCs are familiar with at-home management options and can help you quickly overcome this painful condition.
Resolving Mastitis- When to Seek Treatment
When to go to the hospital for mastitis?
If the symptoms associated with mastitis aren't improving within 12-24 hours of active management and you're unable to see your provider quickly as is often the case at night or weekends, or you become acutely ill, then a trip to urgent care or the ER is warranted.
Can Mastitis come and go?- Recurrent mastitis
If mastitis comes and goes for a short period, occurs in the same breast, or seems that it resolves despite antibiotic use, the cause may be improper treatment or recurrent mastitis.
Not every provider will do a milk culture when mastitis is suspected.
Causes of recurrent mastitis include:
Chronic bacterial Infection
Secondary fungal infection
Breast disease
The treatment of recurrent mastitis will vary depending on the cause. For a chronic bacterial infection that has not resolved with short-term high-dosage antibiotics, a low dose of antibiotics may be required for the duration of lactation.
In cases of secondary fungal infections, the lactating parent and baby require treatment concurrently. Anything that comes into contact with the breast/milk or baby's mouth requires daily sterilization- Bottles, nipple shields, towels, bras, pacifiers, toys, etc. Additionally, partners may too need treatment, especially if there is nipple play during intimacy.
When recurrent mastitis always occurs in the same breast, or there is an unchanging mass (lump) in the breast, breast disease should be suspected, and parents referred to a breast specialist for evaluation.
Which antibiotics are best for Mastitis?
Which antibiotic is best will depend on the type of bacteria causing the infection and the sensitivity of that bacteria. The most common strains of bacterium that cause infectious mastitis produce an enzyme called penicillinase, which reduces the effectiveness of traditional Penicillin.
For this reason,penicillinase-resistant penicillins, such as Dicloxacillin or Flucloxacillin, are often prescribed first. Cephalexin or Clindamycin may be prescribed depending on one's sensitivity to penicillin. Cephalosporins, a more broad-spectrum class of antibiotics, are safe for lactating parents to take but may be used less frequently.
When MRSA is the suspected or confirmed caused of infectious mastitis, Vancomycin or Trimethoprim-sulfamethoxazole (Bactrim) is necessary.
Will Mastitis heal on its own- without antibiotics?
Not all cases of mastitis require antibiotics, and with the growing concern with antibiotic resistance, alternative treatments are preferred as a first-line solution.
First and foremost, regardless of whether or not antibiotics are warranted, YOU MUST CONTINUE TO REMOVE MILK. Milk removal is the most important and effective treatment for all causes of mastitis.
Therapeutic breast massage can help get both your milk and lymphatic fluid flowing, thus speeding up the healing process.
Many parents utilize home remedies such as castor oil compresses, ginger, salt baths, and/or homeopathic remedies such as Phytolacca or Belladonna. Many parents report success with this, though, it's important to note there is no scientific research to support the effectiveness of homeopathic remedies.
Another option, albeit less well-known, is the use of probiotics to resolve mastitis. L. fermentum CECT5716 and L. salivarius CECT5713 have been proven to be an effective alternative to antibiotics. Klair lab's TARGET B2™ contains L. Fermentum and can be used preventively or during an active case of mastitis.
Inappropriate management of mastitis
Improper management of mastitis can lead to complications and premature cessation of lactation/breastfeeding. Some providers, while able to diagnose and treat mastitis, are uneducated about breast physiology and the impact that abrupt discontinuance of breastfeeding can have on breast health.
If your provider suggests that you immediately stop breastfeeding or milk removal in an attempt to resolve mastitis or as a byproduct of the initiation of antibiotics, or if they fail to order a milk culture for persistent mastitis, the recommendation is against all current scientific evidence or mastitis management.
It's also not uncommon for providers to request milk cultures when mastitis is persistent or recurring, despite the recommendation to do so in the Academy of Breastfeeding Medicine Mastitis Guidelines.
Mastitis Complications
Untreated or improperly treated mastitis can lead to serious complications such as:
Premature weaning
Breast abscess
Thrush
Breast Phlegmon
Blood infection (Sepsis)
Necrotizing Fasciitis
Multiple Organ Dysfunction Syndrome
Toxic shock syndrome
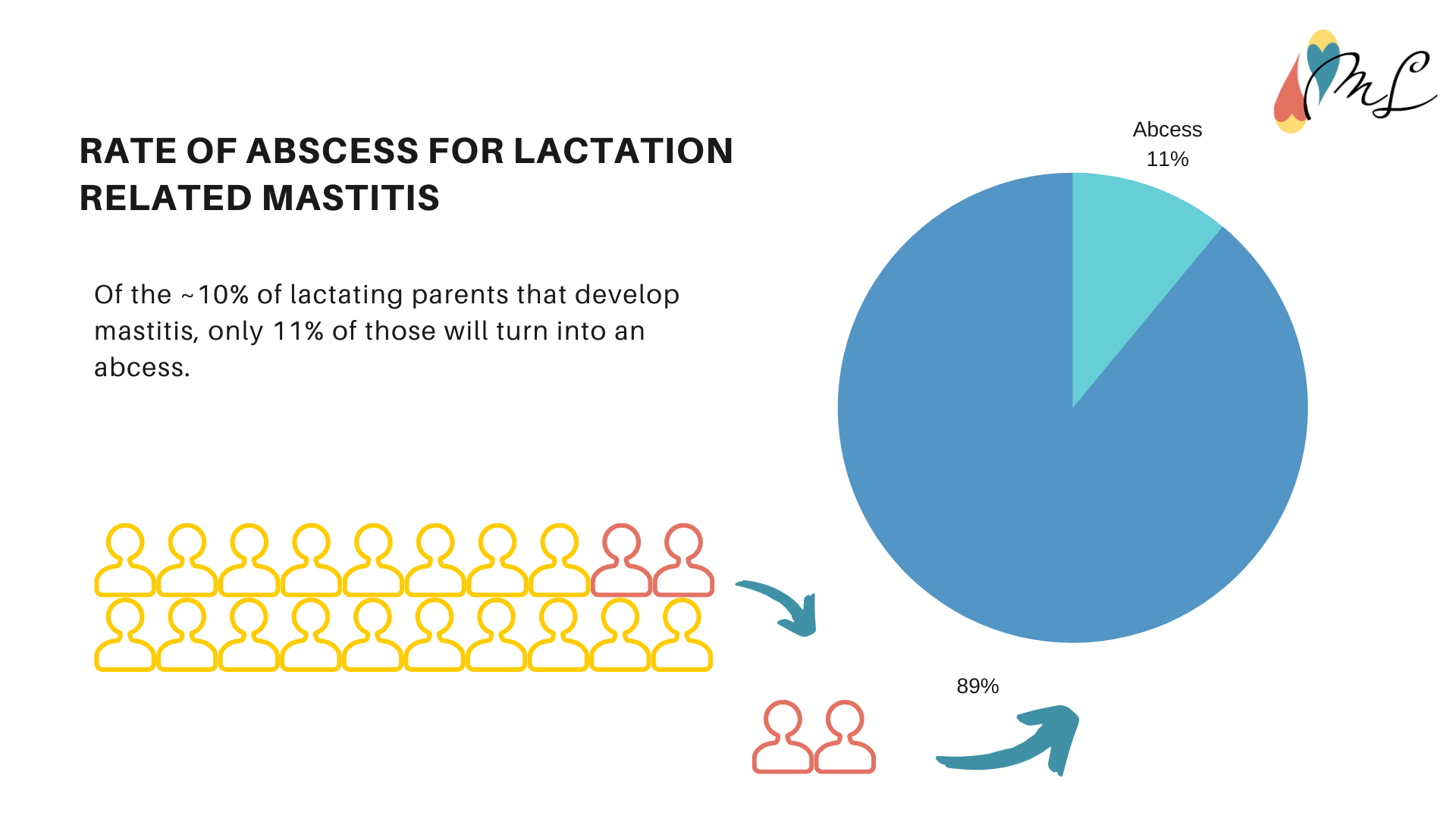
When does Mastitis turn into an abscess?
There is no specific time frame in which mastitis turns into an abscess, but timely management is essential for preventing one from developing. An abscess is a byproduct of your body's attempts to contain the infection - white blood cells (neutrophils) attack the bacteria and dissolves any dead breast tissue creating pus. A barrier of fibrinogen forms around the developing pus pocket, forming an abscess.
The longer the bacteria is present in the breast, the longer that the breast sends out neutrophils to remedy the infection, and the longer liquifying necrosis (pus formation) occurs, the higher the chance of abscess formation.
When does Mastitis get worse?
Mastitis is a quickly progressing condition, and depending on what's the underlying cause and how actively it's managed, it can take a day to weeks to get worse. Subclinical mastitis, for example, may take weeks of an underlying infection to worsen, or it may never turn into acute mastitis. Acute mastitis may eventually turn into suppurative mastitis (such as an abscess) after a prolonged period of ineffective treatment. And one may become acutely ill from mastitis just within days of the first symptoms of possible mastitis.
With proper management and treatment, your mastitis should resolve fairly quickly, without worsening.
Can Mastitis be fatal?
As with any infection, there is a possibility that the bacteria will enter the bloodstream, causing sepsis, which can be fatal. It's estimated that less than 1% of mastitis cases ever turn into sepsis, and of those cases, 60-80% of patients who develop sepsis survive.
Less discussed but equally life-threatening complications of mastitis include Necrotizing Fasciitis, Multiple Organ Dysfunction Syndrome, and Toxic Shock Syndrome. The occurrence of these complications is exceedingly rare, with very little literature on each with regards to mastitis.
Impact of Mastitis on Lactation, Breastfeeding & Pumping
Can my baby drink my milk if I have mastitis?
Continued breastfeeding and expression are encouraged as there is little risk of illness for the average healthy infant. The bacteria that could potentially cause mastitis is often present in your milk whether or not you develop mastitis, and it poses little to no risk to your babies. An acute case of mastitis, even if a bacterial infection is an underlying cause, is not a reason to discontinue breastfeeding.
It may be reassuring to know that during mastitis, some immunological properties typically found in your milk are elevated, and as a result, provide additional protection to your baby.
In rare instances, human milk feeding/breastfeeding may be temporarily interrupted. This situation usually only occurs in cases of MRSA mastitis infection when a baby is premature or ill, and the risk of them becoming ill from being exposed to MRSA is exceptionally high or in cases of severe bilateral mastitis associated with more aggressive pathogens.
Mastitis has been associated with slow weight gain in babies, though the underlying mechanisms are not yet understood. It is possible the slow gaining may be due in part to a decrease in milk supply from that breast, especially if a baby requires both breasts to meet their intake needs. Further research is needed to understand the association between slow weight gain and mastitis better.
I have mastitis, but I can't get milk out!
If you have mastitis but are unable to drain your breast, you are not alone. Many parents struggle with milk removal during mastitis, which is both frustrating and concerning, as milk removal is an essential aspect of mastitis management.
A significant contributor to the difficulties in milk flow is the inflammation, which can decrease the size of the milk ducts. The narrowing of the milk ducts, combined with any physical blockages from accompanying plugged ducts, can make milk removal exceedingly challenging.
Anti-inflammatories, pain meds, warm compresses, cold compresses, and therapeutic breast massage may be needed simultaneously to start milk flow.
Your lactation professional is best suited to help guide you through managing mastitis, getting your milk flowing, and rebuilding your supply.
Why is my baby refusing to breastfeed from my breast while I have mastitis?
Mastitis impacts the taste of your milk by increasing the saltiness of it, as well as elevating the umami/bitter flavors of your milk. Your baby may refuse the milk from your mastitic breast due to the taste, and once the inflammation/infection clear up, they may resume taking your breast as usual.
Mastitis can reduce your milk supply in that breast, further elevating the saltiness of your milk, so if your baby is particularly sensitive to the changes in your milk, they may take longer to resume breastfeeding as anticipated from that breast.
Unusual Mastitis
This post covers the most common forms of mastitis you're likely to experience as a lactating parent, which is mastitis in ONE breast due to inflammation or infection. Below is a brief list of other types of mastitis one could experience;
Nonpuerperal mastitis- a category of inflammatory breast conditions not related to pregnancy or lactation
Zuska's disease- Subareolar (under the areola) abscess and breast duct fistulas that form as a result of keratinization of epithelial cells in the ducts of the mammary gland
Periductal mastitis (Mammary duct ectasia)- widening and thickening of the milk duct leading to the blocking and fluid build-up of the duct. It can lead to bacteria overgrowth and abscess formation. There are four different possible meanings of Duct ectasia, as there are variations and consistency issues with the terminology.
Plasma Cell Mastitis- a variant of periductal mastitis with a prominent plasma cell component of the build-up
Granulomatous Mastitis- a rare chronic inflammatory breast condition with an unknown cause. It may be a secondary complication of a wide variety of diseases such as tuberculosis, sarcoidosis, or diabetes
Granular Lobular Mastitis (Idiopathic Granulomatous Mastitis) - a subtype of Granulomatous mastitis, which presents as inflammatory nodules of the breast. As mentioned above, it is a poorly understood condition.
Comedo Mastitis: A remarkably rare form of mastitis similar to Granulomatous Mastitis but with breast tissue death
Eosinophilic Mastitis: A benign disorder caused by an infiltration of the mammary gland by disease-fighting white blood cells (eosinophils)
Cryptococcal Mastitis- A deep fungal infection of the breast generally seen in cattle, with few reported cases in humans
You may also like: