Is Donor Milk Safe?
Read Time | 8 mins
The past few days, many mainstream news stations have restarted coverage on a tragic situation at Geisinger Medical Center in Danville, Pennsylvania, where three premature babies died, and five other preemies became ill after coming into contact with Pseudomonas bacterium.
In the four weeks that have passed since the initial story broke, investigators have found the cause of the contamination, and as expected, news headlines have progressively gotten more and more focused on the method of contact with Pseudomonas, which was via Donor milk preparation.
Despite no other additional details or updates - the number of ill babies, the bacterium that caused the illness, and the precautions taken after remain the same- the headlines have skewed from unbiased reporting to sensationalism and fear-mongering.
And though I agree that reporting the method of transmission is essential and that, unfortunately, in this case, it was tied directly to the preparation of human donor milk, the headlines have created quite a stir in which parents are asking: Is using Donor milk safe?
Human milk is the optimal food for human babies, even when milk from a birthing or lactating parent (often referred to as Mother's Own Milk) is unavailable.
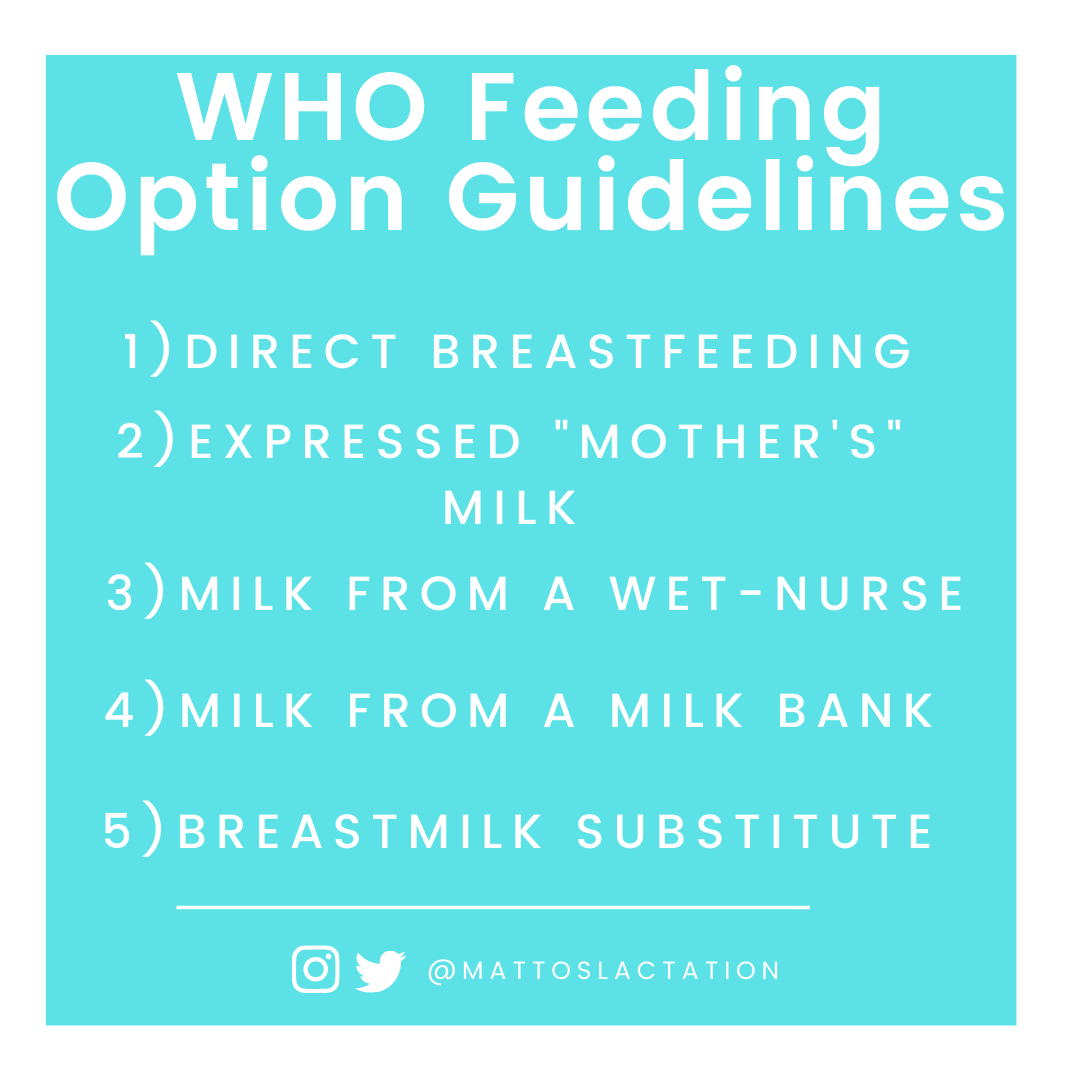
The World Health Organization, who's primary mission and concern is improving public health all across the world, outlines a "hierarchy" of feeding options in a publication titled The Global Strategy for Infant and Young Child Feeding. In this guideline, it states that when direct breastfeeding is not an option, and "mother's" own milk is not available, milk from a wet-nurse or milk bank, should be used before breastmilk substitutes, such as formula.
The benefits of human milk, especially when used in medically fragile populations such as premature babies, are well documented. Postnatal infection rates, specifically the risk of Necrotising Enterocolitis, decrease when human milk is used, regardless of from who it comes.
Unfortunately, however, when it comes to feeding options, it would seem that all methods of feeding babies carry some risk.
And even though the possibility of adverse outcomes from the use of donor milk is not universal and highly dependent on a multitude of factors, tragic stories like this highlight the need for an honest discussion on the benefits and risks of using donor milk.
Note: This whole post focuses on FORMAL milk sharing- that is, milk obtain through a hospital from a milk bank. Milk donation through a milk bank in the United States requires serological (blood) testing, milk culturing, and pasteurization before being used by parents. Additionally, to be offered, providers must write a prescription, which means that generally, only NICU babies get it, as they make up the sickest/earliest babies. The risks of Informal Donation will differ.
RISKS OF DONOR MILK
The most significant risk of Donor milk use is in hospital, post pasteurization contamination.
There are strict policies and regulations regarding donor milk use- both at the milk bank and the hospital-which ensure the health and safety of the babies receiving it.
Unless there is a processing center located in the hospital, most hospitals obtain frozen milk, which must be placed in a commercial freezer at -20 degrees Centigrade (-4 degrees Fahrenheit) until it's ready to use.
There are two main methods used to defrost human milk: Defrosting the milk by submerging the vessel containing the frozen milk in warm water (warm milk bath) or by placing it in a breastmilk warmer. The method used will vary by hospital protocol.
Once defrosted, the next steps pose the most risk of contamination, as most hospitals received milk 3-4 ounce portions, which must be separated into smaller volumes, appropriate for the individual baby's intake needs.
At Geisinger Medical Center, this is where the Pseudomonas bacterium contamination occured, as it was on the equipment used to portion out the milk volumes.
Once thawed, staff must discard any unused pasteurized milk by 48 hours, though commercially sterile donor milk can be stored up to 7 days in a refrigerator.
Another possible risk to donor milk use may be restricted growth of Very Low Birthweight Infants. The connection between infant growth of premature babies and infant feeding is under intense study, and the ideal rate of growth for preemies, both with human milk that is and is not fortified, is poorly defined. At this time, there's not enough information to know what impact, if any, slower growth rates may have on long term outcomes and what mechanisms are responsible for any delays.
One possible cause is that donor milk is comprised of "full-term milk," which is milk from parents who are making milk for their older, often full-term babies. "Full-term milk" has a lower amount of protein, fat, and amino acids compared to "preterm milk"- having less of the properties that preterm babies need to reach their caloric demands.
In other words, parents donating are at a stage of lactation that differs from parents who's babies are currently in the NICU, and this may result in a different rate of growth in some babies.
WHAT ABOUT DISEASE TRANSMISSION?
It might be surprising, but there are very few diseases in which human milk feeding is contraindicated.
Even in those who have HIV, depending on where they live, exclusive breastfeeding may be safer than using a breastmilk substitute, such as formula.
Yet, understandably, parents are often concerned with disease transmission, sometimes so much so, that they will refuse to use pasteurized donor milk in the hospital when they are unwilling or unable to use their own milk.
Milk banks perform pasteurization, a process used to kill bacteria and viruses on all milk before it is distributed to the hospitals. There are multiple methods of pasteurization available, but Milk banks often use Holder pasteurization. Once milk from multiple parents is nutritionally analyzed, cultured, pooled, it is then heated to 62.5 C ( 144 F) for 30 minutes. Immediately after the 30 minutes, it is rapidly cooled then frozen on -20 C.
Additionally, Microbiological cultures are screen by an independent laboratory from batches after pasteurization as an additional safeguard to disease transmission.
I could not find a single case of disease transmission from pasteurized milk from a milk bank.
WHAT ABOUT THE BENEFICIAL PROPERTIES OF HUMAN MILK
Though the search for better pasteurization options continues as pasteurization does impact some milk components, the majority of "goodies" in milk remain in high number, including the essential immunoglobulins and oligosaccharides. Macronutrients are also nearly unaffected- and despite a reduction in number, the biological activity of human milk proteins are preserved after pasteurization.
While I’m talking about the beneficial properties and any reduction caused by pasteurization, I think it’s important to note that when compared to raw donor milk, pasteurizing donor milk may have an impact on the breakdown of proteins (proteolysis), fats (lipolysis) and disintegration of human milk. As with research, the long term effects of this impact remains to be seen.
In short, unpasteurized, unfrozen raw human milk remains to be the ideal for most babies, pasteurization allows medically fragile babies to get MOST of the benefits of human milk without the risks of disease. Still, most importantly, it enables babies to avoid the risks associated not receiving human milk at all.
So IS DONOR MILK SAFE?
Yes.
Pasteurized donor milk is safe for all babies who can tolerate human milk, even with the increased risk of contamination due to hospital practices.
It's of no reassurance to the parents who have lost their lives. Still, fortunately, issues involving donor milk is extremely rare, and often, it's not directly related to the human milk in of itself but rather hospital practices.
The Pseudomonas bacterium, which is generally harmless in healthy populations, is common and is found everywhere from plants to your skin. By nature of serving sick populations, hospitals are high-risk places for contamination and must stay vigilant in reducing illness transmission, especially in at-risk populations.
This situation, serves as a painful reminder that even “harmless” bacteria can cause harm for fragile babies.
WHAT CAN YOU DO?
Prior to utilizing any milk or breastmilk substitute that is prepared in hospital, it's important to ask the following questions:
1) Is there a separate nutrition room in your unit for the preparation of Donor milk, Human milk fortification, or Formula prep?
Donor milk and formula should NOT be prepared bed side.
2) Do you use a laminar airflow hood for preparation?
3) Do you use single-use equipment for Donor milk or Formula preparation?
4) Do you have a Protocol for Donor milk handling and Supplementation I can review?
And most importantly, ensure that you and everyone who handles any feeding devices/equipment (to include pumps & flanges) have proper hand hygiene.
If you haven't already, please follow me on Facebook by liking my page! I would love to have you a part of our growing family!